Resuscitative thoracotomy
** This topic is available as a learning module on Ko Awatea **
Click HERE to access this course
Introduction
A resuscitative thoracotomy performed in the ED or pre-hosptial setting is a procedure of last resort to save a potentially salvageable patient who has suffered a traumatic cardiac arrest.
A meta-analysis performed in 2015, showed a 10.6% overall survival rate in patients with penetrating trauma who had a resuscitative thoracotomy performed, with a good neurological outcome in 90.4%. The most benefit was from stab wounds (15.8%) and less from gun-shot wounds (7.2%). Patients with blunt trauma had a 2.3% survival rate, with a 59.4% chance of remaining neurologically intact.1
Predictors of survival from resuscitative thoracotomy
- Penetrating > blunt
- Single stab wound > GSW
- Thoracic trauma > extra-thoracic trauma
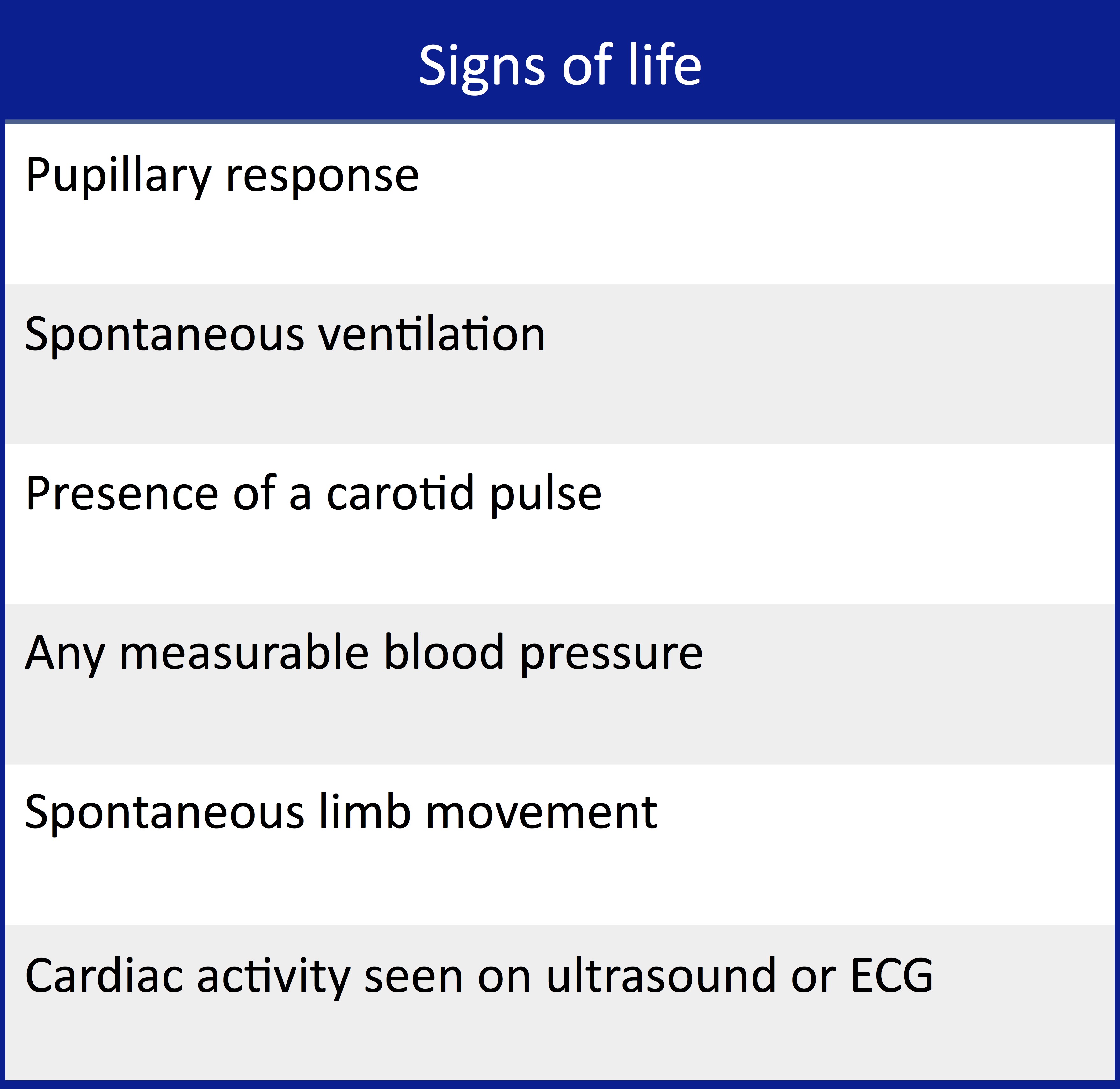
- Signs of life on arrival to ED > no signs of life on arrival to ED
Aims of resuscitative thoracotomy
- Relieve pericardial tamponade and control cardiac haemorrhage
- This is the primary role of resuscitative thoracotomy and has the greatest benefit if successful
- Internal cardiac massage and defibrillation
- Control intrathoracic haemorrhage (eg: pulmonary or great vessels)
- May need to perform a hilar twist or clamp*
- Control air embolism*
- Cross clamp thoracic aorta*
- Preferentially increase blood flow to coronary arteries and brain
- Decrease downstream (eg: abdominal) bleeding
*technically challenging for the non-surgeon and less survival benefit when performed in the ED
Indications
- Penetrating chest trauma with signs of life in the past 10-15 minutes
- The best evidence for survival from a thoracotomy is in patients with a single penetrating stab wound to the chest1,2
- While a resuscitative thoracotomy is primarily performed on patients in cardiac arrest, patients that are peri-arrest with hypotension (SBP <70 mmHg) unresponsive to chest decompression and blood products with penetrating chest trauma could be considered for resuscitative thoracotomy in the ED if an operating room is not immediately available.
- The best evidence for survival from a thoracotomy is in patients with a single penetrating stab wound to the chest1,2
Controversial indications
- Penetrating extra-thoracic trauma with cardiac arrest
- Blunt (thoracic) trauma with signs of life on arrival to the ED who then have cardiac arrest1,2,3
- Note that these injuries are often more complex and not easily treatable by non-surgeons with a resuscitative thoracotomy
- Ultrasound evidence of cardiac tamponade may indicate patients with a potentially favourable outcome
- Note that these injuries are often more complex and not easily treatable by non-surgeons with a resuscitative thoracotomy
Contraindications
- Penetrating trauma with CPR in progress >15 minutes and no signs of life
- Blunt trauma with no signs of life on arrival to ED
- Other injuries incompatible with survival (eg: severe TBI)
Complications
- Injury to patient
- Phrenic nerve transection, injury to lung, coronary arteries, myocardium, oesophagus etc….
- Infection
- Scarring
- Injury to providers
- High risk of blood borne pathogen exposure from sharps, broken ribs etc….
Equipment
- PPE (gown, gloves, eye protection)
- Antiseptic eg: betadine
To open the chest
- Scalpel (20 blade)
- Long blunt dissecting forceps
- Surgical shears or other heavy duty scissor
Ideally
- Rib retractors
- Eg: Finochieto retractors
- Gigli saw
For intrathoracic procedure
- toothed forceps or mosquito forceps (lift pericardium)
- iris scissors
- suture material eg: 3.0 prolene
- stapler
Ideally
- Lung retractor (“whisk” type)
- Aortic clamp
- Lung clamp
The procedure
1. Intubate patient and positive pressure ventilate with 100% oxygen
2. Don PPE
3. Rapidly apply antiseptic solution to chest
4. In the 5th intercostal space, create an incision through the skin and subcutaneous tissue with a scalpel extending anterolaterally from the sternum to past the posterior axillary line.
- If performing a clamshell – a second assistant can do the same on the right. The skin over the sternum should also be incised.
5. With blunt forceps or heavy scissors, dissect down through the pleura going over the rib (to avoid the neurovascular bundle) as if performing a thoracostomy.
- At this entry point, use the scissors to cut through the intercostal muscles and pleura following the skin incision line
- If performing a left anterolateral approach only, now insert rib spreaders to expose the left hemithorax
- If performing a clamshell approach – cut through the sternum to join the left and right thoracic incisions.
- The sternum can usually be cut with heavy duty scissors. If not – a Gigli saw can be utilised.
- Note that the sternum may have some adhesions to the pericardium – these can be gently dissected through with blunt tipped scissors or forceps.
- When the clamshell is completed, rib spreaders can be inserted to open the wound. If no rib spreaders are available, an assistant can lift the freed chest wall.
6. Identify pericardium, lift with forceps and incise longitudinally
- Take care to avoid phrenic nerve
7. Completely open pericardium and deliver heart out of sac
- Scoop out pericardial blood/clot
8. Identify any myocardial laceration and close
- Place finger on laceration
- Can close with sutures or staples
If the main injury is a laceration to the myocardium, this may now result in ROSC
The patient should now be transferred to the OR for formal operative repair
Other interventions
Internal cardiac massage
Grasp heart in hands with wrists opposed and milk heart from apex
Adrenaline can be injected directly into the left ventricle
Internal defibrillation
Using internal paddles – 10J
Control of lung parenchymal bleeding
Clamp site of bleeding, can use mattress sutures to repair
Consider hilar clamping or twist to control severe pulmonary bleeding
This will require transection of the inferior pulmonary ligament
Aortic cross clamping
Aorta will need to be dissected away from the prevertebral fascia posteriorly and the oesophagus anteriorly
Ensure that aorta is clamped, not oesophagus
Click HERE to watch the procedure being performed on a part task trainer
And HERE to watch it on a real patient (viewer discretion advised)
References
- Seamon MJ, Haut ER, Van Arendonk K, Barbosa RR, Chiu WC, Dente CJ, Fox N, Jawa RS, Khwaja K, Lee JK, Magnotti LJ. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the Surgery of Trauma. journal of trauma and acute care surgery. 2015 Jul 1;79(1):159-73.
- Cothren CC, Moore EE. Emergency department thoracotomy for the critically injured patient: Objectives, indications, and outcomes. World Journal of Emergency Surgery. 2006 Mar 24;1(1):4.
- Slessor D, Hunter S. To be blunt: are we wasting our time? Emergency department thoracotomy following blunt trauma: a systematic review and meta-analysis. Annals of emergency medicine. 2015 Mar 31;65(3):297-307.
- Simms ER, Flaris AN, Franchino X, Thomas MS, Caillot JL, Voiglio EJ. Bilateral anterior thoracotomy (clamshell incision) is the ideal emergency thoracotomy incision: an anatomic study. World journal of surgery. 2013 Jun 1;37(6):1277.
Related Guidelines
About this guideline
Published: February 2018
Author: Emma Batistich
Updated: April 2021, May 2024 (Nicholas Longley)
Approved by: Northern Region Trauma Network, Health New Zealand | Te Whatu Ora – Northern Region, NRHL, St. John
Review due: 2 years