Penetrating thoracic trauma
Most commonly occurs from stabbings and gunshot wounds as a result of interpersonal violence. In New Zealand, gunshot wounds are relatively rare – the majority of penetrating chest trauma is from stabbings.
Algorithm for management of penetrating thoracic trauma
pentrating chest trauma flow
Potential injuries
Lung injuries
Pneumothorax – the most common serious injury from penetrating chest trauma. If there is an open connection between the environment and thoracic cavity, an open pneumothorax (aka sucking chest wound) can develop where air can become preferentially entrained into the pleural space, causing ipsilateral lung collapse. If air can enter the thoracic cavity but is prevented from exiting (by tissue valve effect) a tension pneumothorax can rapidly develop
Haemothorax. The source of blood can be from intercostal vessels, lung parenchyma or great vessels/heart (these patients usually have a massive haemothorax and are clinically unstable)
Cardiac laceration/tamponade
Due to its position, the right ventricle is the most commonly lacerated area of the heart. While any penetrating injury to the thorax could cause a cardiac injury, be particularly mindful of stab wounds to “the box” – bound anteriorly by the clavicles, bilaterally by the mid clavicular line, inferiorly by the costal margins.
The “box”
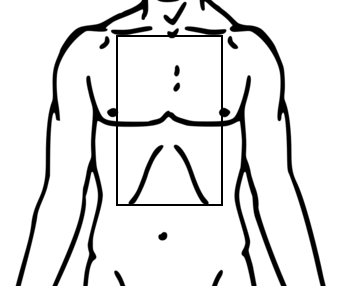
Adapted from: Mikael Häggström (File:Line-drawing of a human man.svg) [Public domain or Public domain], via Wikimedia Commons
A long knife or a GSW/missile could cause a cardiac injury from a more lateral anterior or posterior entry wound.
Great vessels
Most patients with these injuries die prior to presentation to the ED. Consider if the patient has a massive haemothorax with rapid ongoing blood loss after tube thoracostomy insertion
Tracheobronchial injury
Less common in penetrating thoracic trauma
Patients may present with haemoptysis, subcutaneous emphysema of the neck, or tension pneumothorax (or a pneumothorax with persistent large air leak)
Diagnosis is confirmed with bronchoscopy
Oesophageal injury
Can be challenging to diagnose but have high mortality rates if untreated.
Symptoms and signs include – haematemesis, cervical or mediastinal air seen on CXR or CT, a left sided pleural effusion (+/- particulate matter draining from tube thoracostomy)
Definitive diagnosis is made by contrast studies or oesophagoscopy
Diaphragm laceration and intraabdominal injury
Penetrating injuries to lower chest should be considered as junctional wounds as they can cause injuries above and below the diaphragm.
Diaphragm injuries can be very challenging to diagnose – CT scan is only around 82-87% sensitive in detecting diaphragm laceration in penetrating trauma. If this is strongly suspected, direct operative visualisation by laparoscopy or VATS is indicated.
Investigations
CXR
If the patient is haemodynamically stable, a CXR should be performed. Injuries such as a pneumothorax may not manifest on early imaging. A repeat CXR should be performed at 6h.
If a patient is unstable, eFAST can rapidly detect tension pneumothorax, massive haemothorax and cardiac tamponade. In stable patients, eFAST can be used in conjunction with a CXR.
CT
Stable patients with injuries that potentially traverse the mediastinum or diaphragm should be considered for CT scanning.
As the trajectory of a gun shot wound or missile can be unpredictable, most patients with injuries as the result of this mechanism should have a CT scan.
Note that a “normal” CT does not rule out tracheobronchial, oesophageal or diaphragm laceration
Bronchoscopy
For suspect tracheobronchial injuries
Gastroscopy/oesphagoscopy
For suspected oesophageal injuries
Laparoscopy or Video Assisted Thoracic Surgery (VATS)
For suspected diaphragm lacerations
- Accurate trajectory estimation will assist injury identification
- On plain imaging, use a paperclip taped over the skin that is open for posterior wounds and closed for anterior wounds
- The number of wounds (entry/exit) + foreign bodies should be an even number (have a think about this!)
- If not you are…..
- missing a wound
- missing a bullet (expand imaging ie: image the neck, chest and abdo/pelvis)
or
-
- the patient has been shot before (with the FB remaining in situ)
Disposition – interhospital transfer guidelines
Asymptomatic patients with normal vital signs that have a normal initial and 6h CXR (and no concerns about mediastinal, diaphragm, intraabdominal or vascular injuries) can be discharged from ED with advice to return if increasing shortness of breath or other concerns.
penetrating chest injury unstable
penetrating chest stable
About this guideline
First published: February 2018 (Author: Emma Batistich)
Updated April 2021 (Savitha Bhagvan), Oct 2023 (EB), May 2024 (Savitha Bhagvan)
Approved by: Northern Region Trauma Network, Health New Zealand | Te Whatu Ora – Northern Region, NRHL, St John
Review due: 2 years